March 31, 2025
Breakthrough Investigational Medications in Kidney Disease Treatment
Some form of kidney disease affects approximately 35.5 million adults in the United States. The prevalence of kidney problems and the serious impact...
August 29, 2024
5 Educational Strategies to Reduce Vaccine Hesitancy
Vaccine hesitancy came to the forefront during the COVID-19 pandemic, but medical researchers and physicians have been concerned about its implications for...
February 21, 2018
Who Oversees Clinical Trials?
Clinical trials are carefully conducted studies—using human volunteers—which are used to test potential medical treatments with an end goal of receiving an FDA approval for usages in a...
December 14, 2016
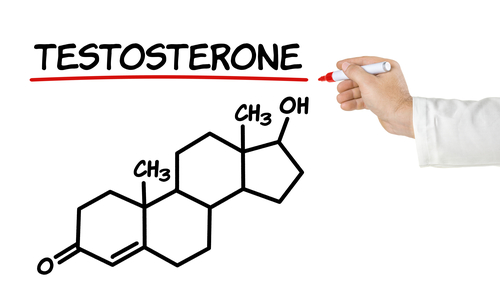
What Causes Low Testosterone Levels?
One in every six American men experiences low testosterone levels. The condition is so common that Low-T (as it’s abbreviated) affects approximately 13-15% of all American men....

November 21, 2016
What is kidney dialysis?
Kidneys are small fist-sized organs on either side of the abdomen that purify blood and help rid the body of waste. You might not be fully aware of the importance of your kidneys; but they play...

November 1, 2016
Clinical Research Toolbox
While Americans face unique health risks, thanks to modern clinical research and medical advancements, our overall life expectancy has increased in the past 100 years. Clinical trial...

October 3, 2016
Five Things You Didn't Know About Clinical Trials
Every year, researchers work with thousands of volunteers to collect new data about medications; and shortly thereafter, new treatments enter the marketplace in part,...

August 30, 2016
How do clinical trials help improve the future of medicine?
Clinical trials are an integral and essential part of the drug development process. Each and every week, researchers across the country work closely with...

July 28, 2016
Inclusionary and exclusionary criteria are specific limitations that clinical researchers place on a recruited study population. Researchers may screen and select specific participants in order to isolate variables that...

June 30, 2016
Clinical trial data helps researchers create new treatments and facilitates innovations in the field of medicine. These studies rely heavily on volunteers, and the data that researchers collect from study participants...