October 28, 2024
Liver Health in High-Risk Groups: What You Need to Know
The term “liver disease” includes several different conditions. Anyone can develop liver disease, but some individuals have a higher risk than others....

October 25, 2023
Five Beneficial Foods and Supplements for Liver Health
A liver that functions at its best is essential to maintaining overall health for people of all ages, especially as you get older.
Perhaps one of the factors...
October 28, 2022
A Look at Current Liver Disease Therapies
Over 100 million Americans have liver disease according to the American Liver Foundation. Unfortunately, most of those patients don’t know they have the condition.
The good...
October 18, 2021
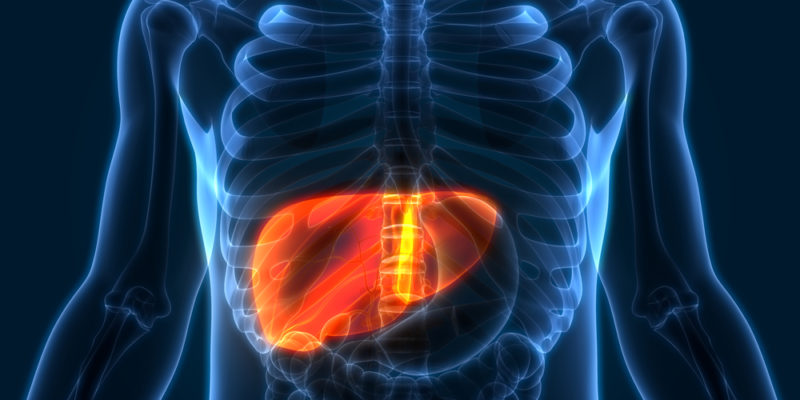
What are the Four Stages of Liver Disease?
The liver performs several crucial functions: it filters toxins from the blood, metabolizes drugs, stores energy, fights infections, and helps with digestion. This...
December 23, 2020
Understanding the Liver’s Role in Digestion
The liver is the body’s second-largest organ, second only to the skin. This approximately 3-pound, football-sized organ plays an important role making sure our bodies are...
November 25, 2020
Five Liver Damage Warning Signs
The liver is football-sized organ under your right rib cage. It is crucial for digesting food and clearing toxic substances from the body. The liver breaks down toxic substances such as...

October 30, 2019
What Causes Liver Cancer?
October is Liver Cancer Awareness Month, which means it’s a good time to educate yourself about one of the deadliest forms of cancer—especially if you or a loved one may be at...
November 30, 2018
Seven Ways to Keep Your Organs Healthy
Sun up to sun down, your body’s organs are working together to keep you healthy. Your liver breaks down harmful substances in your body, excreting that waste into your blood;...

January 31, 2017
Key Risk Factors for Liver Cancer
Over time, behaviors like smoking, heavy drinking and poor health take their toll on the internal organs. The liver is a highly resilient organ, but recurring abuse does take a toll....

September 26, 2016
How Does The Body Metabolize Medication?
Thanks to the diligent work of clinical researchers (and, of course, clinical trial participants), we now have crucial knowledge about how the body metabolizes different types...